Persistent Depressive Disorder (PDD), also known as dysthymia, is a type of chronic depression that lasts for an extended period of time. Unlike major depressive disorder, which may occur in episodes, PDD is characterized by a long-lasting low mood that affects a person’s quality of life and overall functioning. In this article, we will explore the symptoms, causes, and available treatments for Persistent Depressive Disorder.
What is Persistent Depressive Disorder?
Persistent Depressive Disorder (PDD) is a form of depression that lasts for at least two years in adults or one year in children and adolescents. During this period, individuals experience a depressed mood for most of the day, more days than not. While the symptoms of PDD may not be as severe as those seen in major depressive disorder, they can still significantly impact one’s daily life, relationships, and ability to function.
PDD is often underdiagnosed or misdiagnosed because many people with the disorder may not seek treatment or may attribute their symptoms to a personality trait or temporary mood fluctuation. However, it is important to recognize PDD as a serious medical condition that requires professional intervention.
Symptoms of Persistent Depressive Disorder
The symptoms of PDD are similar to those of major depressive disorder but typically less intense. To be diagnosed with PDD, a person must experience a consistent low mood and at least two additional symptoms for the duration of the disorder. These symptoms may include:
1. Chronic Sadness or Low Mood
People with PDD often feel sad, hopeless, or empty most of the time. This mood persists for months or even years, and the individual may have difficulty feeling joy or enthusiasm about things that once brought happiness.
2. Fatigue or Low Energy
Individuals with PDD frequently report feeling tired or lacking energy, even after a full night’s rest. This fatigue can interfere with daily activities, making it hard to keep up with work, school, or personal responsibilities.
3. Low Self-Esteem
Those with PDD often struggle with feelings of inadequacy or worthlessness. This low self-esteem may be pervasive, causing individuals to feel they are incapable or unworthy of success or happiness.
4. Difficulty Concentrating
Concentrating, making decisions, or focusing on tasks may become more challenging for people with PDD. This cognitive difficulty can affect both professional and personal life, contributing to feelings of frustration.
5. Changes in Sleep Patterns
People with PDD may experience either insomnia (difficulty sleeping) or hypersomnia (excessive sleeping). These sleep disturbances can further exacerbate fatigue and impair daily functioning.
6. Changes in Appetite
Changes in eating habits are common in PDD. Some people may lose interest in food and experience weight loss, while others may eat excessively and gain weight.
7. Social Withdrawal
Individuals with PDD may withdraw from social interactions, preferring to be alone rather than participating in activities they once enjoyed. This isolation can lead to further feelings of loneliness and disconnection.
8. Feelings of Hopelessness
A pervasive sense of hopelessness is often reported by individuals with PDD. They may feel as though their circumstances will never improve, contributing to a sense of helplessness.
Causes of Persistent Depressive Disorder
The exact cause of Persistent Depressive Disorder is not fully understood, but research suggests that a combination of genetic, biological, environmental, and psychological factors play a role in its development.
1. Genetic Factors
Genetics can influence the likelihood of developing PDD. Studies show that individuals with a family history of depression are more likely to develop the condition themselves. Specific genes that regulate neurotransmitters (such as serotonin) may also be linked to a higher risk of depression.
2. Biological Factors
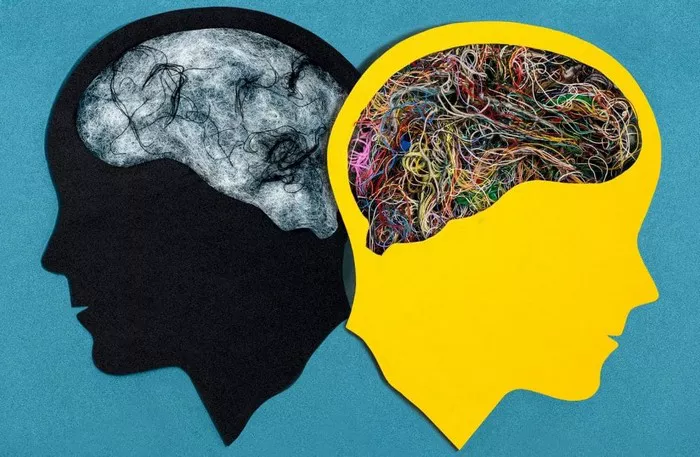
Changes in the brain’s structure and function can contribute to the development of PDD. Neurotransmitters, such as serotonin, norepinephrine, and dopamine, are chemicals that regulate mood and emotions. Imbalances in these neurotransmitters are often found in individuals with depression. Additionally, structural changes in certain areas of the brain, such as the prefrontal cortex, have been observed in individuals with chronic depression.
3. Environmental Factors
Life events such as trauma, loss of a loved one, financial problems, or a difficult childhood can contribute to the onset of PDD. Chronic stress or ongoing difficulties in relationships or work may also increase the risk of developing persistent depression.
4. Psychological Factors
Certain personality traits, such as low self-esteem, high levels of self-criticism, or a tendency to be overly perfectionistic, may make an individual more vulnerable to developing PDD. Negative thinking patterns, such as ruminating on failures or feeling unable to cope with stress, can also contribute to the persistence of depressive symptoms.
Treatment for Persistent Depressive Disorder
Although PDD is a chronic condition, it is treatable. A combination of therapy, medication, and lifestyle changes is often the most effective approach to managing symptoms. The goal of treatment is not only to alleviate the symptoms but also to help individuals build coping skills and strategies to prevent future depressive episodes.
1. Psychotherapy
One of the most effective treatments for PDD is psychotherapy, also known as talk therapy. Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) are two common types of psychotherapy used to treat PDD.
Cognitive-Behavioral Therapy (CBT) focuses on changing negative thinking patterns and behaviors that contribute to depression. In CBT, individuals learn to identify and challenge distorted thoughts and replace them with more realistic, positive ones.
Interpersonal Therapy (IPT) focuses on improving interpersonal relationships and communication. This approach can be helpful for individuals with PDD who experience difficulties in their social or work lives.
2. Medication
Antidepressant medications can be effective in managing the symptoms of PDD. Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and other classes of antidepressants are commonly prescribed to individuals with persistent depression. These medications work by regulating the balance of neurotransmitters in the brain.
It is important to note that medication alone is often not sufficient for long-term management of PDD. A combination of medication and therapy is typically recommended.
3. Lifestyle Changes
Lifestyle changes, such as regular physical activity, healthy eating habits, and sufficient sleep, can significantly improve mood and overall well-being. Exercise, in particular, has been shown to have antidepressant effects by boosting the production of endorphins and other mood-enhancing chemicals in the brain.
Engaging in social activities, practicing mindfulness, and developing relaxation techniques (such as meditation or yoga) can also help alleviate symptoms of PDD.
4. Support Groups
Participating in support groups, either in person or online, can provide individuals with a sense of community and understanding. Sharing experiences with others who are facing similar challenges can reduce feelings of isolation and help individuals learn new coping strategies.
Conclusion
Persistent Depressive Disorder is a chronic condition that can affect many aspects of a person’s life, but with proper treatment, individuals can manage their symptoms and lead fulfilling lives. Recognizing the symptoms and seeking early intervention is crucial to reducing the severity and impact of the disorder. If you or someone you know is struggling with PDD, it is important to reach out to a healthcare professional for an evaluation and appropriate treatment options.
You Might Be Interested In:
-
How to Increase Intimacy and Communication with an Avoidant Partner: 15 Ways
-
Dismissive Avoidant Attachment Style: Causes, Traits & Healing