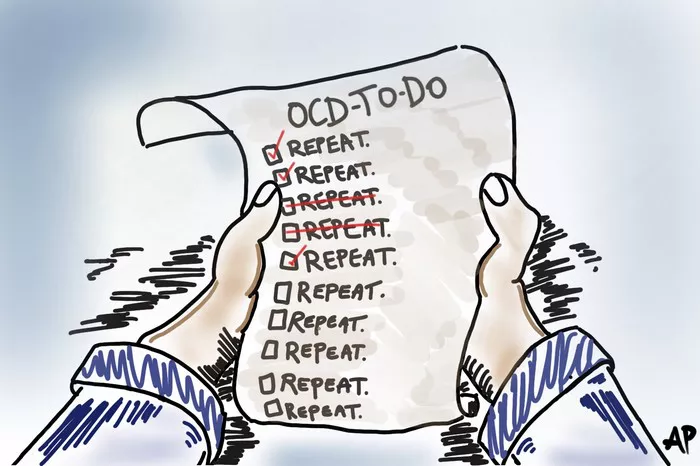
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by persistent and intrusive thoughts (obsessions) and repetitive behaviors (compulsions) that individuals feel driven to perform. Many people wonder whether OCD can simply disappear over time. While some symptoms may lessen or change in intensity, OCD is generally considered a chronic condition that requires management. In this article, we explore whether OCD can go away on its own, factors that influence symptom severity, and treatment options that can help individuals regain control over their lives.
Understanding OCD: A Lifelong Condition?
OCD is classified as a chronic condition, meaning it often persists throughout a person’s life. However, its severity and impact can fluctuate over time. Some individuals experience periods of remission, where their symptoms become minimal or manageable, while others struggle with persistent and severe compulsions.
Can OCD Naturally Fade Away?
In rare cases, some people experience a decrease in symptoms without formal treatment. This can be due to various factors, including changes in environment, stress levels, or brain chemistry. However, OCD does not typically disappear on its own, and untreated OCD can worsen over time. Even if symptoms become less severe, the underlying thought patterns and compulsions often remain.
Childhood vs. Adult-Onset OCD
OCD can develop at any age, but it most commonly appears in childhood or early adulthood. Studies suggest that children with mild OCD symptoms may outgrow certain compulsions as they mature. However, for most people, OCD remains a lifelong condition, even if it goes through periods of dormancy. Adults who develop OCD later in life are less likely to see spontaneous remission and usually require treatment to manage their symptoms effectively.
Factors That Influence OCD Symptoms
While OCD is typically a long-term condition, several factors can influence the severity and progression of symptoms:
1. Genetics and Brain Chemistry
OCD has a strong genetic component, and individuals with a family history of OCD or related disorders may be more likely to experience chronic symptoms. Neurotransmitters, particularly serotonin, play a significant role in OCD, and imbalances can contribute to persistent symptoms.
2. Stress and Life Events
Stressful events, trauma, or major life changes can trigger or exacerbate OCD symptoms. Some individuals may notice that their symptoms fluctuate with stress levels, becoming more manageable during calm periods but worsening during high-stress situations.
3. Coping Mechanisms and Personality Traits
People who have strong coping skills or naturally lower anxiety levels may find that their OCD symptoms are less disruptive. On the other hand, perfectionistic tendencies and high anxiety can make symptoms more severe.
4. Access to Treatment and Support
Those who seek treatment—such as therapy, medication, or lifestyle changes—often experience significant improvement in their symptoms. Support from family, friends, or support groups can also make a difference in managing OCD.
Treatment Options for Managing OCD
While OCD may not completely go away, effective treatment can significantly reduce symptoms and improve quality of life. Several approaches have been proven to help individuals manage their condition:
1. Cognitive Behavioral Therapy (CBT)
CBT, particularly a form called Exposure and Response Prevention (ERP), is the most effective treatment for OCD. ERP involves gradually exposing individuals to their fears and preventing them from engaging in compulsive behaviors. Over time, this helps retrain the brain to resist compulsions and reduce anxiety.
2. Medication
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for OCD. Medications such as fluoxetine, fluvoxamine, and sertraline help regulate serotonin levels and reduce obsessive thoughts and compulsions. Some people respond well to medication alone, while others find that a combination of therapy and medication works best.
3. Mindfulness and Stress Reduction Techniques
Practices like mindfulness meditation, deep breathing, and progressive muscle relaxation can help individuals manage anxiety and intrusive thoughts. While these techniques are not a cure, they can complement other treatments and improve overall well-being.
4. Lifestyle Changes
Regular exercise, a healthy diet, and adequate sleep can positively impact mental health. Reducing caffeine and alcohol intake may also help, as both substances can contribute to anxiety and compulsive behaviors.
5. Support Groups and Community Resources
Connecting with others who have OCD can provide a sense of understanding and encouragement. Support groups, whether in-person or online, offer valuable resources and coping strategies.
Can OCD Ever Be Cured?
Although OCD is considered a chronic condition, many individuals achieve long-term remission with the right treatment and management strategies. “Cure” may not be the correct term, but many people with OCD reach a point where their symptoms no longer interfere with daily life. Some individuals may have only mild, manageable symptoms that do not require ongoing treatment.
Signs That OCD Is Under Control
- Reduced frequency and intensity of intrusive thoughts
- Ability to resist compulsions without extreme distress
- Improved ability to function in daily life without OCD-related disruptions
- Decreased reliance on compulsions for anxiety relief
Final Thoughts
While OCD does not typically disappear on its own, it is a highly treatable condition. With proper therapy, medication, and self-care, individuals can achieve significant symptom relief and lead fulfilling lives. If you or someone you know is struggling with OCD, seeking professional help can make a crucial difference in managing the condition effectively.
You Might Be Interested In: